21 OLD MALE WITH ALTERED SENSORIUM
MEDICINE E LOG BOOK
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Chief complaints:
Pt came to casualty in state of altered sensorium with slurring of speech since yesterday
History of presenting illness :
Pt does hotel management and stays alone.
He was apparently asymptomatic 5 days back. He had fever 5 days back which was high grade, continuous, associated with chills and rigors. No history of cold and cough . He went to local hospital got treated but the fever did not subside.
Later after a day he consumed beer, had biryani.
He had 1 episode of vomiting and loose stools since 3 days. (2 days back), while he was in room suddenly he had involuntary movements of all 4 limbs associated with frothing, uprolling of eyes, post ictal confusion, he bit his lower lip no tongue bite . He had 1 episode of vomiting at the time of involuntary movement, and loose stools.
Loose stools, foul smelling.
Since yesterday afternoon, pt was in altered sensorium , with slurred speech, and deviation of mouth.
He was presented to hospital on 19/09/22 and was treated he was sedated at 1am was sent home at 4:30am . He woke up at 2pm . He had altered sensorium and involuntary movements.
No c/o weakness of upper limb and lower limb.
No h/o cough, cold, palpitations, syncopal attacks, chest pain
PAST HISTORY
N/k/c/o - DM, HTN, EPILEPSY,TB , ASTHMA
FAMILY HISTORY
No significant history
PERSONAL HISTORY
appetite- normal
Diet- mixed
Bowel and bladder - normal
Sleep- regular
Habits - alcohol consumption occasionally,
Smoking
General examination:
On examination:
Pt is in altered sensorium
No pallor, Icterus, clubbing, cyanosis lymphadenopathy, edema
VITALS
BP-110/70mmhg
PR - 85bpm
RR -16 cpm
Temp. 100°F
CVS S1, S2 +
RS - BAE +, NVBS
Per abdomen - soft and non tender
CNS EXAMINATION:
NERVOUS SYSTEM EXAMINATION
a. Conscious
b. Not Oriented to time, place and person
c. Speech and language –no aphasia, dysarthria, dysphonia
d. Memory – immediate-retention and recall, recent and remote - not intact
MOTOR examination
Meningeal signs
Kernigs sign +
Brudzinski sign -
Power:
Rt. Lt
UL +4/5. -4/5
LL. +4/5. -4/5
Tone
UL. N N
LL. N. N
Hand grip: 100%. 100%
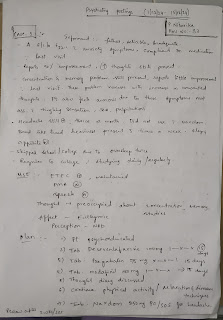
Provisional Diagnosis : Altered sensorium under evaluation 2° to dengue encephalitis with pre renal AKI 2° to acute gastroenteritis.
Investigations
Treatment








Comments
Post a Comment