A 24 year old male with vomiting, sob and blood in urine
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDERS
A 24 year old male daily wage labourer came to the OPD with a
CHIEF COMPLAINTS of decreased urine output , vomiting since 9 days .Difficulty in swallowing and oral ulcers since 8 days .
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 9 days back then he developed severe vomitings due to an excessive binge drinking without any consumption of food. The vomitings were 4-5 episodes/day and were non bilious, non blood stained, non foul smelling, watery and occurred immediately after consumption of food or liquids. Also complaints of difficulty in swallowing since 8 days.
Patient developed oral ulcerations later that day. He was taken to a local hospital where medication (mouth wash and some gel for ulcers). was provided and did not get relief. 5 days ago he had complaints of shortness of breath (Grade 3) and decreased urine output with blood in the urine.And went to a private hospital and endoscopy was advised and blood tests were done in which increased serum creatinine levels and bilirubin levels were detected and referred to our hospital and got admitted for dialysis. 4 days ago the patient was observed to develop a white coating in the mouth and over the tongue( dermatology opinion taken).
He has no H/o fever, loose stools, pedal oedema, pain abdomen, burning micturition, cold, cough .
PAST HISTORY:
No similar complaints in the past
No H/o HTN, diabetes, asthma, epilepsy and tuberculosis.
PERSONAL HISTORY:
Diet: mixed. Appetite: normal
Bowel and bladder: irregular.
Sleep: adequate.
Addictions : alcohol consumption since 4 yrs daily( around 180 ml) (binge drinking episode 2 days back before onset of present symptoms ) and paan occassionally.
Allergies: none.
Family history: not significant
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative moderately built and nourished
Vitals
Temperature: afebrile. PR: 83bpm
RR: 22cpm. BP: 140/90mmHg
Pallor: absent
Icterus: present
Clubbing: absent
Lymphadenopathy: absent
Oedema : absent
SYSTEMIC EXAMINATION:
Per abdomen: soft on palpation, bowel sounds heard, no distention present.
Respiratory system: no wheeze heard, no crepitus heard, normal vesicular breath sounds heard
CVS: S1 S2 heard, no additional murmurs
CNS: no focal neurological deficits.
INVESTIGATIONS:
31/12/22:
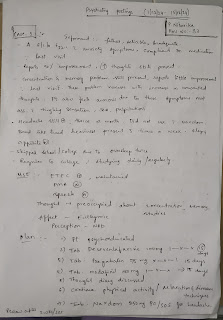
Hemogram
.jpeg)



































Comments
Post a Comment