1801006128 -LONG CASE
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
A 55 year old male who was a daily labourer , was brought to medicine opd with
chief complaints:
•Shortness of breath since 7 days
•Decreased urinary output since 7 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 year back then he developed bilateral pedal edema which was on and off in nature(since 1 year) and was present up to ankle and was pitting type.
For this he visited a hospital and he was on conservative management. He was diagnosed with hypertension and started medication .
On the sunday (12/3/23)night around 12am he had an episode of shortness of breath of class 4(NYHA)which was sudden in onset and gradually progressive, associated with Paroxysmal nocturnal Dyspnea and orthopnea.
No history of chest pain , sweating, palpitations.
No history of cough, hemoptysis
Urine output is decreased,
narrow streamlined urine.
No history of burning
micturition , fever.
During his stay in hospital he has undergone dialysis 4 times.
DAILY ROUTINE :
He wakes up around 5 am in the morning and does his household chores , goes to work for 5 to 6 hrs and returns back home around lunch time 1pm and take rest for the day. He will have his dinner around 7 30 pm and goes to sleep at 9 pm. He now has stopped his daily work since a year.
PAST HISTORY :
Known case of hypertension since 1 yr and on medication
Not a known case of diabetes, asthma , epilepsy, Tuberculosis , CAD.
No Similar complaints in the past.
Treatment history:
Drug history:
Tab TELMISARTAN 40mg OD since 1 year
NSAIDS : taken since 4 years occasionally but from past 2 years taken almost daily for knee pains.
Past surgical history :
No past surgical history
FAMILY HISTORY :
No significant family history
PERSONAL HISTORY :
Appetite - Normal
Diet - Mixed
Sleep - adequate
Bowel habits - regular
Bladder habits - decreased
Addictions - history of smoking (beedi 4 per day since he was 20 years old ), history of alcohol consumption (since 30 yrs and occasionally whisky 90 ml each time since past one year ).
GENERAL EXAMINATION :
(Consent was taken)
Patient is conscious, coherent and cooperative.
Moderately built and moderately nourished.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing- absent
Lymphadenopathy- absent
Edema - bilateral lower limb edema , pitting type , seen in ankle region.
VITALS :
Temperature - Afebrile (98.6F)
Pulse rate - 80 bpm
Blood pressure - 130/80 mm Hg
Respiratory rate - 17 cycles per minute
SpO2 - 95%
SYSTEMIC EXAMINATION :
CARDIOVASCULAR SYSTEM:
*INSPECTION :
Shape of chest : normal
No sinuses, scars and engorged veins.
Mild rise in JVP
No Precordial bulge
No visible pulsations
Apical impulse : not well appreciated on inspection
*PALPATION-
Apex beat: Shift to 6th intercoastal space lateral to midclavicular line
No Parasternal heave and thrills
*PERCUSSION :
Left heart border - not confined with in normal limits
Right heart border normal in location
*AUSCULTATION :
S1 , S2 heard. no murmurs.
RESPIRATORY SYSTEM:
*INSPECTION :
Trachea - midline
Shape of chest - elliptical and bilaterally symmetrical.
Type of respiration : abdomino thoracic
Bilateral airway entry Present
No chest wall defects
Presence of a healing, crusted ulcer on the right hemithorax medial to nipple.
Movement of chest is symmetrical on both sides
No sinuses / scars
*PALPATION :
All the inspectory findings are confirmed
Trachea - central
Chest expansion - symmetrical
Chest circumference - 34 cms
No Tenderness over the chest
*Percussion:
Tactile voacl fremitus:
Right Left
Supraclavicular R R
Infraclavicular R R
Mammary R R
Inframammary R R
Axillary R R
Infra axillary R R
Supra scapular R R
Infra scapular R R
Inter scapular R R
AUSCULTATION :
Vocal resonance
Left Right
Supraclavicular R R
Infraclavicular R R
Mammary R R
Inframammary R R
Axillary R R
Infra axillary R R
Suprascapular R R
Infrascapular R R
Interscapular R R
Breath sounds wheeze heard
CNS EXAMINATION:
1. Higher mental functions:
a. Conscious
b. Well Orientation to time, place and person
c. Speech and language – normal
d. Memory – immediate-retention and recall, recent and remote are present.
Motor system: bulk and tone are normal
Power is 5/5 in all 4 limbs
Deep tendon reflexes are present and normal
Superficial reflexes are present and normal
No involuntary movements
Cerebellar signs absent
Signs of meningeal irritation - absent
Per abdomen examination:
*INSPECTION -
shape of abdomen is normal
No scars and sinuses
Umbilicus is central
*PALPATION -
No Tenderness on superficial palpation.
Temperature - Afebrile
Liver is Non Tender and not palpable
Spleen is Not palpable
*PERCUSSION - tympanic note heard
*ASCULTATION- Bowel Sounds Heard
PROVISIONAL DIAGNOSIS :
Heart failure associated with hypertension.
INVESTIGATIONS:
*Hemogram:
Hemoglobin - 7.7 gm/dl
Total count - 14,100 cells/cumm
Lymphocytes - 16%
PCV - 23.1 vol%
*SMEAR :
RBC - Normocytic normochromic
WBC - increased count (neutrophilic leucocytosis)
Platelets - adequate
*Kidney function test:
Serum creatinine - 4.0 mg/dl
Blood urea - 95mg/dl
*ABG :
PH 7.43
Pco2 - 31.6 mmHg
Po2 - 64.0 mmHg
HCO3 - 21.1 mmol/l
*Urine examination :
albumin ++
sugar nil
pus cells 2-3
epithelial cells 2-3
Red blood cells 4-5
Random blood sugar - 124 mg/dl
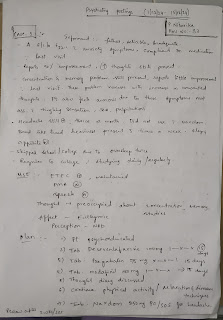
*CHEST X RAY :
*Electrocardiogram :
2d echo:
Final diagnosis:
Heart failure with AKI on CKD 2° to NSAID abuse with hypertension.
TREATMENT :
Ryle’s feed : 100 ml milk with 2 scoops protein powder 4th hourly and 100 ml water 6th hourly.
Inj. Thiamine 100mg in 50 ml NS TID
Inj. Piptaz 2.25g IV TID
Inj. LASIX 40mg IV BD
Inj. Erythropoietin 4000IU SC Once weekly
Inj. PAN 40 mg IV OD
Tab. Nicardia Retard 10mg RT BD
Tab. Metoprolol 12.5mg RT OD
Cap. BIO D3 RT OD.
Hemodialysis
Nebulisation with Duolin 8th hourly and Budecort 12th hourly
Intermittent CPAP
Allow sips of oral fluid
Monitor vitals.












Comments
Post a Comment